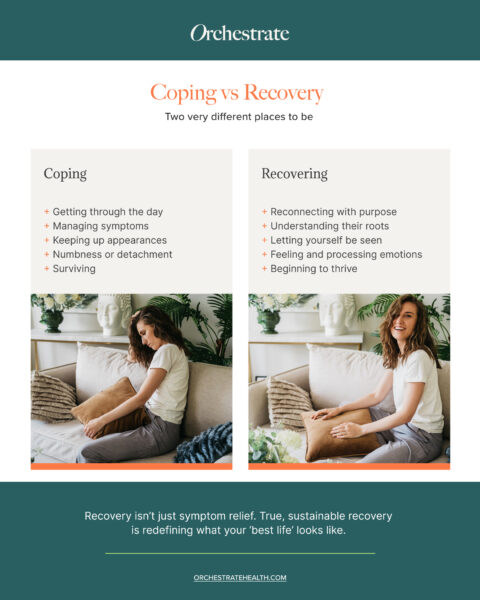
There’s a quiet, often unspoken difference between coping and recovering. And in mental health care, that distinction matters deeply. For some, even those who are actively engaging with support, life can continue to feel like a performance of stability rather than a genuine return to self. From the outside, they may appear to be doing well … attending appointments, taking medication, getting through the day. But internally, the struggle often persists, masked by routines that offer containment but not true resolution.
This isn’t rare. One study found that 53% of individuals who had initially recovered through psychological therapies experienced a relapse within a year – with the majority occurring within just six months1. For those living with depression, around 60% will experience symptoms again in future episodes2. Broader estimates of relapse across anxiety and depression suggest rates as high as 72%3. Even in cases of schizophrenia, relapse remains the norm, with up to 80% of individuals experiencing recurrence within five years of treatment4-5.
That’s why we believe mental health recovery must reach beyond surface-level improvement. Real progress involves both understanding and addressing what lies beneath. In private mental health care, our role is to help bridge that quiet gap between coping vs recovery, guiding each individual toward something more lasting.
What Does It Mean to ‘Cope’?
Coping, in its simplest form, is how we try to manage stress and, in the context of mental health, that can mean anything from pushing through the workday to distracting ourselves from overwhelming thoughts. It’s a widely studied area in psychology6, with over 400 styles of coping identified7, though most are grouped into two main types: problem-focused and emotion-focused coping6.
Problem-focused strategies involve taking action to eliminate or address the root of the stress, such as planning, problem-solving or directly removing the stressor7-8. Emotion-focused strategies, by contrast, are about softening the emotional impact – using distraction, avoidance, rumination or resignation when the source of stress feels immovable7. While both are common, research suggests problem-focused coping tends to be more effective in reducing distress and promoting long-term emotional resilience9, whereas emotion-focused coping may increase the risk of stress-related physiological illness10.
Coping can be essential, especially during acute distress. But it’s not the same as recovering. Managing symptoms may alleviate discomfort in the short term, but does not necessarily restore wellbeing or address the root causes of psychological distress11-12.
The challenge is that coping can look deceptively like progress. Individuals might be functioning well – attending sessions, taking medication – yet feel no emotional shift. And when they still don’t feel ‘better,’ shame or confusion can settle in. This is where even well-meaning coping strategies in mental health can mask ongoing suffering.
Coping is not failure – but it’s not the end point, either.
What Does It Mean to ‘Recover’?
Recovery is often misunderstood as a fixed destination … something you reach once symptoms subside. But for most people, particularly those navigating complex or long-standing challenges, mental health recovery is a far more personal, evolving process.
As Mental Health UK notes, recovery can mean different things depending on the individual12. For some, it’s the absence of symptoms12. For others, it’s learning to manage them in a way that restores confidence, regains control, and enables them to live the life they want12. There may be periods of progress and setbacks, but what matters most is the return of something meaningful.
True recovery involves more than symptom relief. It’s the quiet reappearance of self. Feeling like yourself again. Reconnecting with others. Processing difficult emotions in a way that feels safe. Understanding not just how you cope, but why certain strategies evolved in the first place and which ones continue to serve you.
Importantly, it’s about thriving after treatment, not just surviving it. As Mental Health UK reminds us: whatever it is that’s important to your recovery, you don’t have to figure it out alone12.
This is where long-term mental health support becomes essential; recovery is about building a life that feels possible again, and then walking alongside each person as they begin to live it.
Why this Distinction Matters – And What to Watch For
Sometimes, individuals appear to be doing everything right; attending sessions, taking prescribed medication, maintaining a routine. But something isn’t quite shifting. Progress feels flat and, beneath the surface, a quiet distress lingers.
This is where the gap between coping and recovering becomes particularly important to recognise. Signs might include emotional detachment, a sense of apathy, shame for not improving more quickly, or a subtle sense of despair that’s hard to articulate. In these moments, people often start to feel that they’re performing wellness, rather than truly experiencing it. Going through the motions, but still feeling unwell.
For healthcare professionals or concerned family members, these patterns can be easy to miss. But recognising emotional distress in this form is vital. It’s not a failure on the part of the individual. Rather, it suggests that their current support may not be reaching the depth they need.
Our team specialises in bridging these mental health treatment gaps by offering care that goes beyond symptom management. Our approach is flexible, personalised, and deeply collaborative. We meet each individual exactly where they are, and stay with them until they can begin to move forward with confidence.
How Mental Health Treatment Can Bridge the Gap
Moving from coping to recovering requires more than just a treatment plan. It really calls for a depth of care that meets each person where they truly are.
This begins with trust.
It begins with the time and space to ask difficult questions and with an approach that treats the individual, not the symptoms.
Effective mental health care cannot be standardised or time-limited. To support truly sustainable progress, personalised care must explore the underlying causes of distress, not just manage its surface presentation. It must integrate the physical, psychiatric, and emotional, understanding that each layer contributes to how a person survives and, eventually, how they might begin to heal.
That’s why we centre our work around these principles.
Our at-home mental health treatment offers privacy, discretion, and one-to-one attention, delivered by a multidisciplinary team that wraps around each person, providing a consistent thread of support. Our nurse-led programmes ensure continuity and clarity, while our stepped care mental health model allows support to evolve with the individual’s needs over time.
Importantly, this kind of care is especially valuable for those who can’t, or aren’t able to for whatever reason, access traditional inpatient services; for some, the idea of leaving home is unworkable and for others, visibility carries risk. Our model of community-based care ensures they don’t have to choose between safety and support.
In every case, recovery begins with understanding what that word means to the individual – and being willing to build a team around that definition.
Rediscovering What Recovery Really Means
Recovery is rarely linear. And it’s not always obvious from the outside. The real markers of progress are often internal. They’re quieter, slower, and deeply personal. For some, it might look like feeling safe enough to be honest. For others, it’s reconnecting with meaning, or letting themselves feel again without fear.
This is why, when care focuses only on function, it can miss the heart of the matter. As professionals or loved ones, the question isn’t just “Are they managing?”, but ought to be “What does thriving look like for this individual?”
At Orchestrate Health, we believe that every wellbeing journey must go beyond coping, and that effective mental health support helps people move not only through symptoms, but toward something more lasting.
Recovery isn’t just relief from symptoms. It’s the process of rediscovering who you are, and building a life that feels possible again.
References
- https://www.york.ac.uk/news-and-events/news/2017/research/more-than-half-of-mental-health-patients-relapse/
- https://evidence.nihr.ac.uk/alert/talking-therapies-may-prevent-relapse-of-depression/
- https://www.sciencedirect.com/science/article/pii/S0890856722002441
- https://jamanetwork.com/journals/jamapsychiatry/fullarticle/204795
- https://psychiatryonline.org/doi/full/10.1176/appi.ajp.161.3.473?view=long&pmid=14992973
- https://www.sciencedirect.com/topics/psychology/coping-strategies
- https://pubmed.ncbi.nlm.nih.gov/12696840/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4565746/
- https://link.springer.com/article/10.1023/A:1020641400589
- https://pubmed.ncbi.nlm.nih.gov/23148818/
- https://institutemh.org.uk/research/nottingham-ms-research-group/symptom-management
- https://www.mentalhealth.org.uk/explore-mental-health/a-z-topics/recovery